UCI Lab Works Toward Creating Tissue-Engineered Heart Valves
April 10, 2025 - Dr. Arash Kheradvar’s lab at UC Irvine is developing improved options for heart valve replacements. Every year, over five million Americans are diagnosed with heart valve disease and over 100,000 patients get heart valve replacements, according to the Centers for Disease Control and Prevention.
Current valve replacement options are not ideal: mechanical heart valves require patients to take blood thinners while valves made from animal tissue, such as those derived from cows or pigs, usually last only about 10 years. Kheradvar, a UCI professor of biomedical engineering, believes that creating a hybrid tissue-engineered heart valve, derived from a patient’s own cells and cultured over a permanent scaffold, will offer a long-lasting biocompatible solution.
He said his work is like creating a cyborg, much like the character in The Terminator. “Arnold Schwarzenegger was a robot covered by human flesh. We’re doing the same thing with heart valves,” Kheradvar explained. His hybrid tissue-engineered heart valve combines patient-derived cells with a nondegradable polymeric scaffold. “This approach merges the advantages of both mechanical and biological valves, mimicking the biocompatibility and hemodynamics of a native valve, while potentially offering the long-term durability of a mechanical valve,” he said. “The leaflets of the hybrid tissue-engineered valve are made from an ultra-thin polymeric scaffold that will seamlessly integrate into the patient’s tissue once the valve is implanted.”
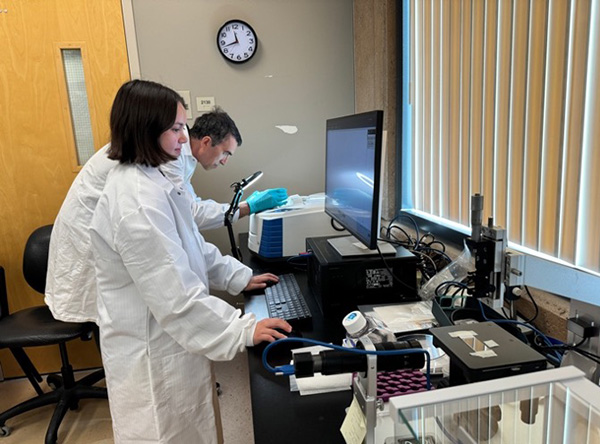
Kheradvar’s latest research introduces new findings on a material made from polycarbonate-based polyurethanes, which they intend to use for the valve scaffold. These polymers are often utilized in other implantable medical devices as well. Their journal article was recently published in Royal Society of Chemistry Advances. The paper details the material properties and biocompatibility of two polycarbonate-based polyurethanes, providing critical insights for potential valve scaffold applications.
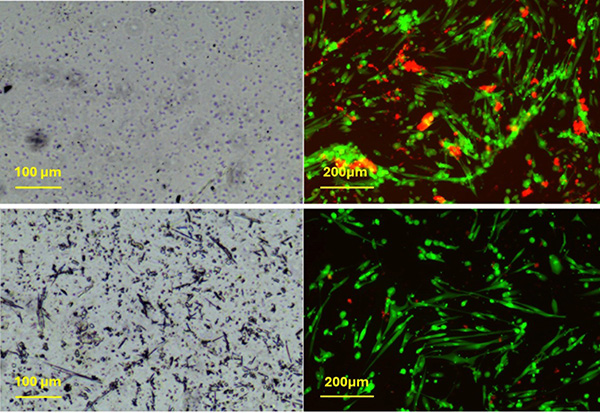
For this project, Kheradvar’s research team included senior scientist Farhad Sadeghi, postdoctoral scholar Yasaman Zamani, and biomedical engineering junior Kaylee Bear. Kheradvar speaks highly of Bear who joined his lab as a freshman. “She's really excited about our research and is extremely motivated and thorough. I have high expectations for her.” Bear who is a co-author on the paper says she has enjoyed being part of the lab. “I’ve learned a lot about research writing and how to make the polymer solutions that get casted in films and are tested for material characterization.”
Zamani explains the team’s findings: “Our goal was to characterize two polymers and evaluate how cells react to them.” The cytotoxicity tests demonstrated that both polycarbonate-based polyurethanes (PCUs) maintained over 70% cell viability, confirming their suitability for medical use. Additionally, Sadeghi mentioned that “polycarbonate-based polyurethanes offer better oxidative stability and lower degradation rates compared to other polyurethanes, making them a more reliable choice for long-term implant applications.” These findings have implications for a variety of medical devices.
Looking ahead, their next step is to conduct open heart surgery in animals. The researchers plan to test the biocompatibility of their scaffold in sheep. Kheradvar’s ultimate goal is to develop patient-specific heart valves, so patients may never need a valve replacement again.
- Natalie Tso